A developmental disability diagnosis can hit hard — but it isn’t a knockout
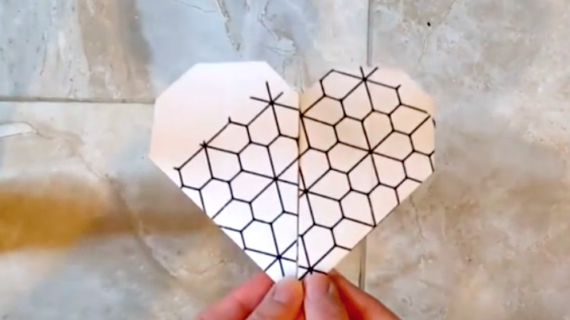
Photo above of Artemis displaying her drawings by Stephanie Strasburg/PublicSource. Story by Rich Lord.
Artemis knows her shark facts, is learning Spanish and draws colorful cats, upside-down, that practically leap off the page when she turns them right-side-up.
At age 7, she’s doing well in school, but her early classroom experiences were rocky. Standing in line, staying in her seat and understanding personal space didn’t come easily. Kindergarten teachers tried to track behaviors and sent home behavior charts with more frowny face stickers than smiles.
Artemis’ mother, Maribeth Hamel, worried about the message that was sending to Artemis, then 5. “We would change all of the frowny faces to smiley faces” at home, said Maribeth.

Maribeth, of Brookline, didn’t know that she could ask for accommodations at the Pittsburgh school without a diagnosis. Maribeth is diagnosed with attention deficit hyperactivity disorder and Artemis’ father, Donald Doherty is a neuroscientist who believes neurodiversity enriches humanity — but both know that labels have consequences.
“I was worried about the impact of an autism diagnosis,” said Maribeth. “There is so much stigma around this.”
Some people wear labels including “autistic,” “ADHD” and “neurodivergent” proudly, and there’s a growing push for awareness. But people who think and act differently are still among the last picked for the team in school, accepted to college and hired into the workforce.
An evaluation for disability can feel like a double-edged sword. Yes, it opens the door to services. But it also cements that status and can prompt a shockingly rapid reevaluation of a loved one’s future.
The term “disability” implies difficulty with conventional employment. Federal data indicates that less than half of people with disabilities are employed, and many of those with jobs are part-timers. The increase in disability diagnoses has implications for the workforce and economy of the future — not to mention the hopes and dreams of individual households.
Maribeth and Donald opted to have Artemis evaluated at age 5. Not long into the session, the evaluator “just basically blurted out that she was autistic,” Maribeth recounted. The evaluator’s only real advice, Maribeth said, was to let Artemis delve into her interests.
“Artemis was playing with Legos off to the side and hearing people talking about her,” Maribeth said. Easily forgotten when kids are different: “Children are listening very, very intently.”
At home, the family processed the experience. “She said, ‘I don’t want to be autistic,’” Maribeth recounted. “I said, ‘Artemis, you are still you. This doesn’t change who you are.’”
More developmental disability diagnoses
The Centers for Disease Control and Prevention estimates that around one in six kids have developmental disabilities, including attention deficit hyperactivity disorder, autism, cerebral palsy, hearing loss, fragile x syndrome, Tourette syndrome and other conditions. Nationally, the prevalence of those diagnoses has steadily increased.
Prior to 2017, Allegheny County did not register children with autism diagnoses. Since then, the number of children registered with the county’s programs for intellectual disabilities and autism has settled in at around 800, out of around 226,000 minors in the county.

The number does not reflect all children diagnosed, as many families stop short of registering with the county while their kids get most services through schools.
The county catches more adult autism and intellectual disability diagnoses because people ages 18 and over may need county services. The number of adults registered has risen gradually, from around 5,400 in 2017 to around 5,800 last year.

Nationally, increases in developmental disability diagnoses are often attributed to improved awareness and the broadening of diagnostic criteria for some conditions, and current estimates are still viewed by some as an undercount.
A long wait for a diagnosis
A child with an undiagnosed disability may be at a long-term disadvantage.
“Early identification and intervention for developmental disorders are critical to the well-being of children,” according to Jennifer Zubler, a pediatrician with Good Samaritan Health Center in Atlanta and an executive committee member of the American Academy of Pediatrics Section on Developmental and Behavioral Pediatrics.
Screening for developmental delays is supposed to occur when a child is 9, 18 and 30 months old, with additional inquiries for signs of autism at 18 and 24 months, Zubler said. But those screenings don’t always happen — even when the pediatrician has the best of intentions.
“Most of my patients don’t have a stable medical home,” she said. “They don’t come for well-child visits, which is when a screening is supposed to be done. … They will come with three or four kids, they may be unable to complete the [pre-visit] form” or screening forms.
Pediatricians screen for signs of autism, but are just beginning to be encouraged to diagnose that condition in the pediatric office, said Zubler. Other conditions typically require referrals to specialists when a screening identifies risks, and most pediatricians still refer patients with indications of autism to specialists and early intervention.
That can take a long time.
Karen Lucarelli, of Spring Hill-City View, took her son for his three-year checkup in March 2023 and was told he should get an evaluation for developmental disability, due to his extreme dietary pickiness and lack of progress toward potty training. She said she called UPMC Children’s Hospital of Pittsburgh and was eventually given an appointment date — in October 2024.
The day before the appointment, her son started using the toilet.
After two hours of conversation and play, “they basically just gave me a paper” saying her son’s problems weren’t severe enough to warrant a diagnosis “and sent me on my way.” She said she’s glad that the evaluator was “cool with where he is,” but disappointed that she won’t get help with the challenges with which she’s been grappling.
UPMC declined multiple requests for an interview for this story and did not provide requested specifics on the length of waiting lists for evaluations. “The Child Development Unit at UPMC Children’s Hospital provides timely and comprehensive neurodevelopmental evaluations for children up to age 7,” spokeswoman Andrea Yorchuck wrote, adding that families can receive services “after a thorough intake assessment tailored to the specific needs of the child and family.”
“Just getting diagnosed is very hard” because of the wait for an appointment, said Dr. Gary Swanson, a psychiatrist with Allegheny Health Network, who has been evaluating young patients for 30 years.
Pediatricians can diagnose many developmental disabilities, but often prefer to refer patients to specialists, said Swanson. He said relatively few physicians are trained in gold-standard tools like the Autism Diagnostic Observation Schedule, leading to long waits. “It may take a year for you to be evaluated, which is a very long time if you’re seeing a 3-year-old and you have concerns.”

Mary Wildman, vice president of Autism Pittsburgh, said parents call her organization frequently, looking for guidance on how to get an evaluation sooner, saying they’re on numerous waiting lists. “Six months seems to be typical,” she said.
After diagnosis come Medical Assistance/Medicaid applications, program waiting lists and school processes that cost still more time.
“It feels like a lot of hurry up and wait,” said Noor Pervez, community engagement manager for the Washington, D.C.-based Autistic Self Advocacy Network.
From genetic testing to ‘life span’ care
At the University of Washington in Seattle, the push for early diagnosis has led to expanded use of genetic testing.
“There really is very much of a change toward trying to push the genetic testing earlier and earlier and broader and broader,” said Dr. Dan Doherty, interim head of the university’s Pediatric Division of Developmental Medicine. While there are no definitive lab tests for some developmental differences — including autism — there are for numerous other conditions. A genetic test can sometimes “make a huge difference” in finding the right intervention, he said.
The shortcoming: A genetic diagnosis doesn’t necessarily come with a specific therapy that has a high likelihood of effectiveness, Doherty said. “Of the thousands of genetic neurodevelopmental conditions, there are high-value therapies for a very small number.”
A definitive, scientific diagnosis, though, can provide a sense of certainty and alleviate concerns that loved ones somehow inadvertently injured the child, said Doherty.
Whether it comes from a lab test or a conversation, the moment of diagnosis can be tough on households, said Dr. Bethany Ziss, a developmental and behavioral pediatrics practitioner at Allegheny Health Network.

“I get a lot fewer parents who are devastated by the diagnosis now than I did a decade ago,” said Ziss, noting that she gets many of her referrals from people who affirm neurodiversity. Sentiments may be different in broader society. “More generally, research suggests that parents today are more negative about autism than they were several decades ago, even though the diagnostic criteria have actually widened to include people with less impairment.”
Her approach is to be “very cognizant that I don’t want to come in and present this as bad news.” Instead she frames the path forward in positive terms. “Here’s some strategies you can try. Here’s some things the teachers can do. … Or here’s some books, here are some websites.”
Ziss wants people to leave her office with an action plan starting the next day. That’s not something every pediatric evaluator provides.
“Some people in my field do assessments only,” Ziss said. “You get ‘em in, you give them diagnoses, you give them some resources, you wave.”
Dr. Dennis Kuo believes the pediatrician’s responsibility to a person with a developmental disability should go far beyond the diagnosis, extending to “a life course approach.”
Kuo, chief of the Developmental and Behavioral Pediatrics Division at the University of Rochester Medical Center, said URMC’s clinic connects households to family navigators and social workers, guides them to a library of materials they can browse, answers the phone when they call with questions and stays involved with the patient long term. “Can we expect that an institution will still be looking at planning [with the household] in 10, 20 years?” Kuo asked, hypothetically. “The answer is: Absolutely yes.”
‘It shouldn’t be a lottery’
While a diagnosis can feel inherently limiting, Susan Adelman encourages a patient’s loved ones to say “yes” to the young person’s ambitions.
“I had a kiddo who was born with Down syndrome,” said Adelman, an occupational therapist and co-director of the University of Washington Medical Center’s Families as Mentors program.
“My kiddo wanted to be a cheerleader,” Adelman continued. “My kid got to have that real-life experience. … Did they invite her to any parties? No. Did she spend a lot of time with them in high school? Absolutely.”
Now Adelman’s daughter has what the mom calls “a great job” as a lab and office assistant at a biotech company.
“How did it happen?” Adelman asked, hypothetically. “The luck of the draw,” plus showing up at a program that placed her with a successful company, plus the benefit of the doubt that comes “because she is white and speaks English and came from the right side of town.”
“It shouldn’t be a lottery,” said Adelman.
Going into Artemis’ evaluation, Maribeth Hamel worried that she’d emerge with heightened uncertainty about her daughter’s future. “That was part of the trepidation that made me worry about the evaluation,” the mother said. But after the evaluation, “I shifted to concern about how she was perceiving herself.”
Maribeth introduced Artemis to books about autism. Donald views neurodiversity as an evolutionary necessity, and recommended the TV series “Extraordinary Attorney Woo” about a young woman on the autism spectrum. Artemis took to it.
“She just became so excited and proud talking about how she was like Attorney Woo,” said Hamel. The autism spectrum suddenly seemed brighter. “She got to a point where she was kind of proud of it.”
Coming soon: Getting ready for adulthood with a developmental disability.
Rich Lord is Z’s father, and the managing editor of PublicSource, and can be reached at rich@publicsource.org.
Pittsburgh-area resources:
- Allegheny County Department of Human Services Office of Developmental Supports
- Bethany Ziss, M.D., developmental-behavioral pediatrics at Allegheny Health Network
- Gary Swanson, M.D., psychiatry at Allegheny Health Network
- UPMC Children’s Child Development Unit
- The Children’s Institute
- Wesley Family Services
- Watson Institute
- Autism Pittsburgh
- Pittsburgh Public Schools Program for Students with Exceptionalities
- Community College of Allegheny County Disability Resources and Services office
- Pennsylvania Office of Vocational Rehabilitation
- Commonwealth Technical Institute at the Hiram G. Andrews Center
- Penn State WorkLink program
- The Education Law Center
- The PEAL Center
- Pittsburgh Commission on Human Relations
- PA Human Relations Commission
- Autistic Self Advocacy Network
- Trying Together
This article first appeared on PublicSource and is republished here under a Creative Commons license.