Autism support in Pittsburgh: Where to go, what to ask and much more
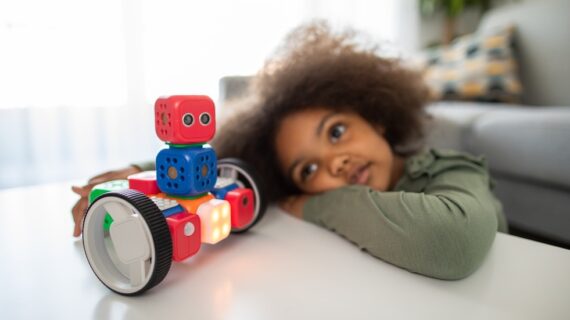
Photo above of a teacher and student in an Autism Support Classroom by Josh Franzos courtesy of the Children’s Institute.
April is Autism Awareness Month, and for many, it’s more than just a month on the calendar. It’s a reminder of their ongoing journey, challenges and triumphs. This journey, shared by many, begins with a simple question: “Where do we start?”
Well, you’re not alone. A lot of parents are in the same boat, wondering where to start and how to get the best support for their kiddos.
Kidsburgh interviewed two experts in the field — Dr. Stephanie Fox, a Licensed Psychologist specializing in autism at UPMC Western Behavioral Health’s Center for Autism and Developmental Disorders (CADD), and Dr. Jessie Northrup, an Assistant Professor of Psychiatry at the University of Pittsburgh School of Medicine — to get their perspectives. Below, they shine a light on critical aspects of autism, offering parents actionable advice and empowering them with the knowledge to navigate this path with confidence and clarity.
What are the common signs or symptoms of autism spectrum disorder (ASD) that parents should be aware of?
Jessie: Autism is diagnosed based on two core areas of symptoms: Differences in social communication, such as trouble with back-and-forth interactions, limited use of nonverbal communication (eye contact, gestures, facial expressions), and social interactions (difficulty understanding social relationships, trouble making and keeping friends with same-age peers). The other is restricted/repetitive behaviors and interests, like repetitive speech, play, or motor movements, sensory sensitivities or sensory dysregulation, intense and specific or uncommon interests, and preference for routine and sameness.
Stephanie: Some common early warning signs of autism include limited interest in social games like peek-a-boo, reduced eye contact, limited social smiling, less frequent vocalizing to others, not showing things to others, not using pointing or other gestures to communicate, lack of responding to their name, limited interest in other infants or toddlers, hand flapping or other repetitive body movements, and repetitive or atypical play with toys.
Can you explain the diagnostic process for autism and what parents can expect?
Stephanie: The diagnostic process can be lengthy! It entails an initial referral to a clinic that specializes in autism and developmental disabilities, followed by an assessment with a psychologist or other behavioral health provider. A gold standard assessment for autism should include, at minimum, a comprehensive interview with the child’s caregiver and administration of a diagnostic test for autism – the most common of which is the Autism Diagnostic Observation Schedule, Second Edition (ADOS-2). More thorough assessments also include assessment of the child’s developmental skills or cognitive ability, assessment of the child’s adaptive functioning, and administration of standardized caregiver and teacher questionnaires. After the assessment is completed, the caregiver can expect to have a conversation with the evaluator to review the results of testing and recommendations for supporting their child.
Jessie: One thing that parents should know to expect, unfortunately, is waitlists. It is likely a good idea to get on a few different waitlists to have a good chance of getting in to see someone. Local waitlists for testing can be as long as six months to one year. Another consideration is many clinicians (especially pediatricians) might be hesitant to diagnose autism in a very young child (before 2 years, especially), even though reliable diagnosis can sometimes be made as early as 18 months. Therefore, it is important to find an expert who is comfortable working with infants and very young children, if you are concerned about a youngster in this age group.
What are some misconceptions about autism that you often encounter, and how do you address them?
Stephanie: There are many misconceptions about autism! Many people assume autistic people don’t have an interest in being social or having friends. Though autistic people might sometimes struggle to make friends effectively, they often have strong social motivation and interest. People also assume children with autism can’t have good eye contact; though lack of eye contact is a common symptom of autism, it is only one symptom among a long list of behavioral features. I have encountered many parents who initially were told their autistic child wasn’t on the spectrum “because they make good eye contact.”
Jessie: Other misconceptions about autism have been precipitated by depictions of autistic people in movies and on television. Not everyone with autism has “savant” characteristics or extraordinary skills, like in “Rain Man.” Not everyone with autism is emotionally distant, like in “The Good Doctor.” And not everyone with autism has an intellectual disability.

How can parents support their child’s development and well-being after receiving an autism diagnosis?
Jessie: This is a great question. It’s really important to remember that your child is still your child! The diagnosis might give you helpful information about what kinds of support they might need, but does not fundamentally change who they are. Remember that not all differences are deficits, and that supporting your child’s development doesn’t have to mean forcing them into being someone they are not.
Stephanie: Consider the recommendations provided by the clinician who diagnoses your child, but ultimately decide which recommendations to follow based on what works for your family and your child. The caregiver is the expert on his or her child!
Are there specific therapies or interventions that are particularly effective for children with autism?
Jessie: I would recommend that parents think about the particular challenges their child is facing and look for interventions to address those challenges. That could be speech therapy to help with language development, occupational therapy to help with daily living skills or sensory challenges, or behavioral interventions if struggling with particular behavioral challenges.
Applied Behavioral Therapy is pretty universally the recommended and offered therapy for autistic children. Many parents and autistic individuals feel that ABA is helpful and there is research to suggest it can improve communication and daily living skills. That said, it is also important for parents to know that a lot of autistic adults report having had really bad experiences with ABA as a child, particularly when therapy used punishment or focused largely on making the person seem less autistic, like forcing eye contact or making someone stop stimming. It might be helpful for parents to understand the controversy around ABA, so they can make their own decisions about what they are comfortable with.
Stephanie: Parents should be aware of the strategies being used in therapy, so they can use these strategies at home or in other environments. Therapy does not only have to happen in an office or with a behavioral health professional; especially when working with a young child, therapy should be comprehensive, consistent, and fun!
What advice do you have for parents in terms of navigating the educational system and advocating for their child’s needs?
Stephanie: This can be difficult! Though there is a federal law to ensure children with autism have access to free appropriate public education (Individuals with Disabilities Education Act; IDEA), the system is not intuitive and can be extremely hard for families to navigate. Consider self-educating on the rights of your child or enlisting an educational advocate through an agency like the PEAL Center. Ask the provider who diagnosed your child whether they can write a recommendation to share with the local public school system about the potential benefits of an Individualized Education Program (IEP) evaluation. Another tip is to not be afraid to ask for what you think your child needs! Meetings with school special education teams can be overwhelming, with groups of school staff and other professionals talking in jargon or unclear language. The team ultimately is there to support your child, so do not be afraid to ask for clarification or provide ideas for supports. Ask the school team, “What kind of things have you done before to help with this challenge?”
Are there any resources or support networks you recommend for parents who are new to the autism community?
Jessie: The number one resource I recommend is learning from autistic people. You can find a lot of resources created by autistic adults online. The Autistic Self Advocacy Network, which is run by autistic adults, has a guide for parents that is freely available online. Other parents with kids on the spectrum can also be a great resource and source of support. Finding support groups or local organizations that organize inclusive spaces and events can be very helpful.
Can you discuss the importance of early intervention for children with autism and how it can positively impact their outcomes?
Stephanie: There is so much science showing the benefits of early intervention (that is, providing therapies within the first few years of life). These benefits are likely related to brain plasticity or the ability of the brain to change and rewire more easily early in development. Some well-documented positive outcomes of early intervention include improved language and communication development, stronger pretend-play skills, improved adaptive skills, and overall stronger social communication (e.g., stronger imitation skills, more frequent shared attention, and more consistent social responding). One thing to keep in mind, though, is if your child has received a later diagnosis or did not participate in early intervention, you haven’t missed the boat! Though we know there are benefits of early intervention, we continue to learn more about the benefits of intervention at all stages of life! Many folks are being diagnosed later in life (even well into adulthood) and there are many highly effective interventions for all ages and ability levels.
What are some key strategies or tips for promoting communication and social skills in children with autism?
Jessie: This is a big question, and there are a lot of different answers. One strategy I like a lot (from a naturalistic developmental behavioral intervention called the Early Start Denver Model) is the strategy of stepping into your child’s spotlight. This is a way of trying to promote and increase positive interactions and communication opportunities with your child by identifying what is capturing their attention, and then finding a way to be a part of that activity or interest. You are following their lead and creating opportunities for connection, rather than trying to pull them into an activity of your choosing. This can be a really powerful way of using your child’s interests to connect and then building off their strengths to develop new skills.
Here are some programs and resources for autism support in the Pittsburgh area:
UPMC Programs:
- Therapeutic Early Autism Program: Intensive intervention for ages 2-5.
- Early Intensive Behavioral Intervention Program: Community-based services.
- Conroy Intensive Treatment Program: Collaboration with schools.
- Partnership with UPMC Children’s Hospital: Comprehensive care, including therapy and support.
AHN Mental Health Services:
- Comprehensive Psychiatric Evaluations are available for children ages 6-18 offered at Psychiatry and Behavioral Health Institute (PBHI) at Jefferson Hospital and at North Fayette Health + Wellness Pavilion.
The Children’s Institute Programs:
- Applied Behavior Analysis (ABA) Services: Holistic support for ages 18 months to 21 years, including therapy and parent training.
Other Local Resources:
- Friendship Circle
- Autism Urban Connections
- Autism Connection of PA
- PEAL Center
- Evolve Coaching
- Pace School
- Spectrum Charter School
Also: PBS Kids recently released the game “Cousin Hodie Playdate,” created by Fred Rogers Productions and Curious Media to be a low-pressure way for children to practice recognizing and identifying their own big feelings and those of their peers. Designed in partnership with experts, the game keeps neurodiverse children top of mind.