
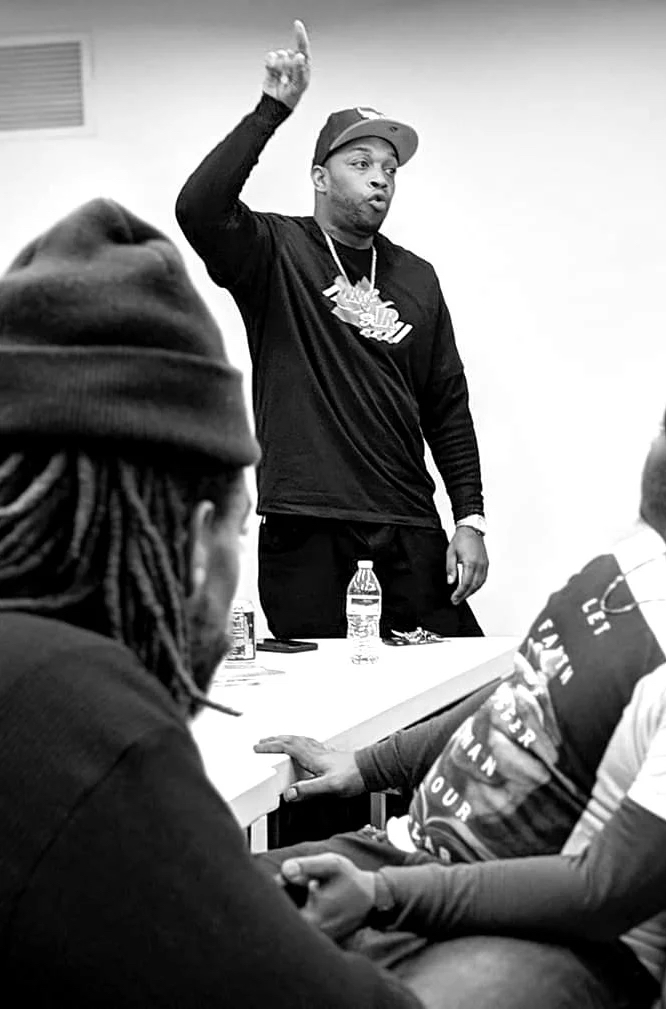
Guest editor Julius Boatwright on community mental health and how we can help young people be well
Photo above by Dan Meyers used by permission via Unsplash.
The world is talking about mental health in new ways. World-class athletes are sharing their mental health journeys, schools are teaching social-emotional skills, and teens are speaking out about the stress they face. In cities and towns around America people are asking: How do we help young people to be mentally healthy and well?
Here in Pittsburgh, Julius Boatwright has been grappling with that question for many years. He is the founder and CEO of Steel Smiling, where a mental health workforce development program called Beams to Bridges equips Black adults with the knowledge and skills to serve as community mental health workers.
This month, as Kidsburgh puts a spotlight on the subject of mental health, we asked Julius to join us as our guest editor. Below, he shares thoughts on how community members can support one another and how parents can support their children.
KIDSBURGH: At Steel Smiling, you have community members and leaders playing an important role in sharing resources, reducing stigma and supporting the mental health of children, youth and families in Pittsburgh’s Black community. Tell us about the two-year training program that helps them do this work.
JB: So far, there are 22 graduates from our workforce development and training program. Throughout the pandemic, the entire group that started the program in September 2019 has stuck together. They’ve gotten the skills, the confidence and the tools to not just support their own mental health and wellness needs, but to go out and support their neighbors and people in their communities. When they’re out and about at work, or in schools, or at places of worship — anywhere they’re out and congregating with others — they’re keeping an eye out for people who might be showing some signs and symptoms related to mental health challenges or mental illness.
KIDSBURGH: When they see these signs, how do they help?
JB: They’re using their active listening skills. And they’re using their empathy and compassion to be able to have conversations with folks. They acknowledge what people are going through, and then serve as a bridge. They don’t provide therapeutic treatment, but they are a bridge to help get someone connected to an appropriate level of care.
KIDSBURGH: For many years, people were uncomfortable asking for support with mental health. As more people seek mental health care, is that stigma going away?
JB: There’s still a lot of stigma, stereotypes and negative generalizations. But over the past 18 months to two years, we’ve turned a corner. The question now is access, and what does quality access look like for folks? We have more people who are saying that they have mental health challenges. We also have more people emerging who define themselves as mental health professionals. Now that more people are seeking treatment, we need to make sure that we’re connecting them with the appropriate level of professionals. Not everyone is going to benefit from just seeing a therapist once a week for an hour. It’s similar to physical healthcare. There are hundreds of medical professionals; you wouldn’t recommend that your primary care doctor give someone a root canal.
Seeking mental health support for yourself or your family? Check out Kidsburgh’s Guide to Community Mental Health Resources.
KIDSBURGH: As people seek out the right mental health professional for themself or their family members, where does peer support fit in the picture?
JB: Communities tend to be very reactive when it comes to mental health. If someone passes away, or there is some community violence, mental health professionals are brought in to talk with people, because kids aren’t coming to school or teachers are struggling. How do we get in front of that? How do we organize and structure, so that collectives of people are meeting in school-day settings or corporate settings or nonprofit spaces for peer support. We need this ongoing engagement, and in my experience, it’s not expensive and not difficult to pull together. It’s just something we need to incorporate into our plans.

KIDSBURGH: Is peer support something that teens and young adults tend to seek out?
JB: Yes. And it’s important to know that mental health and therapeutic support looks and feels different for younger people. You and I might have this mindset of, “We need to just get this young person into therapy.” But that may be like Step Four of a five- or six-step process. Step One might be some sort of informal group with other young folks, or giving them an opportunity to do some creative expression. Any time I’ve seen young people do creative stuff, the mental health stuff comes out. They start talking about their home life. They start talking about some of the challenges they deal with or about the loss of friends. All those things that we define as mental health. One great example is Gwen’s Girls. They activated their young folks and are doing this podcast where teenagers are talking about mental illness and how they go to therapy. The podcast is their creative outlet, and they are educating and destigmatizing. And it’s just them. No parents there. It’s just these young Black girls that are talking about mental health. It’s a tool to kind of help on their mental health journey. I point this out because as adults, we have to give young people the opportunity to navigate the spectrum of their healing journey. It may not look the same as what we’d recommend. We see behaviors, we see signs and symptoms, and sometimes the knee-jerk reaction is “Get him in therapy, get him in therapy, get him in therapy.” But often even we, as adults, don’t just dive right into therapy. We have to go through some sort of journey to get there.”

KIDSBURGH: That’s such good advice. Parents want so badly to take good care of our kids and make sure they’re mentally healthy, and we may not always be sure how to do that.
JB: It’s true. And part of the way we can help them is to give ourselves the space and the grace to ground ourselves. We’re typically the ones, at least 75% of the time, connecting a young person with support. Whether we’re like, “Hey, here’s a phone number” or “Hey, did you talk to the counselor at school?” or “Hey, are you interested in therapy?” We’re often that bridge. So how do we ground ourselves throughout that process? Because if we’re not grounded, if we are not emotionally regulated, and we’re not able to think with clarity, then we may not be able to make the right kind of recommendation. Or we may not be able to model how to support someone when they’re going through a mental health challenge or crisis. Our kids see that and can feel that. So it’s up to us to be well and stable and have a clear mind. Parents and caregivers often think they have to put themselves last. But if we don’t take care of ourselves, then maybe we respond in a way that’s fueled by emotion, and not necessarily coming from a grounded place.
KIDSBURGH: Is this something your team talks about at Steel Smiling?
JB: Arguably the biggest learning that came about through our training program was that a great majority of our people have children and are caregivers. Many are also tending to elderly parents or they’re coaches, mentors, pastors or youth program leaders. Every single person has this self-sacrificial belief: “It’s my duty to put everything above me.” And I have been one of these people. I have celebrated that thought process. And I still struggle with it today. However, we’re trying to raise people’s awareness, especially in the Black community, to say, “Not only is it OK to take care of you. It’s actually critical to take care of yourself, if you want to be effective in taking care of other people. It’s like that old adage. On an airplane, put your mask on first. When we’re all together and that challenge arises, and we’re all struggling for oxygen, you have got to put your own mask on first. If you don’t, you literally won’t be able to help anyone. This moment requires us to slow down in situations that don’t often lend themselves to slowing down. Because we’re in a global crisis, everything feels urgent. We almost feel like we can’t slow down because everything’s so heavy and so layered and complex. But that’s why I would encourage folks to slow down even more.”
KIDSBURGH: If people are interested in mental health support for themselves or their families, where might they begin?
JB: There are a number of different mental health and behavioral health resources throughout Allegheny County. You can do a Google search, or ask on social media, or even ask somebody you know. Often people will make recommendations. Once you’ve found those resources, the next step is navigating those processes. Some people need support with that. The barrier may be financial: Some folks who were once employed are now either unemployed or underemployed, so they don’t have the appropriate level of insurance or income to pay for mental health treatment. Many people need help getting from “OK, I want or need support” to actually getting connected with that treatment. Peer support can help with that.
KIDSBURGH: What do you see when you look toward the future of mental health care?
JB: I think the future is really, really bright when it comes to mental health and wellness. I smile every day when I read an article or I see something on TV saying “So and so gave money to this mental health cause” or “This celebrity shared their diagnosis and is talking about mental health.” We’ve never seen anything like this before. So many people are speaking out and so many mental health causes are getting support. So, once we get through this awakening and we get the right type of resources, then at that point it will just be “Alright, how do we maintain and stabilize what is now the norm?” Healing and mental health will be the norm in schools and workplaces, and places of worship, and everywhere. At some point, it’ll seem surprising if someone doesn’t have a therapist. We won’t be shaming people if they don’t have a therapist, but we’ll be like, “You don’t have a therapist? Wait a minute. We’re going to get you connected with a mental health professional, because this is just what we do.”








